Investigations
We will need to take a full medical and social history. This will include a gynaecological history, details about previous pregnancies and their outcomes, previous contraception used. It is important we take a full history from both partners and it is most helpful if you attend the appointment together.
Female examination and investigation
The doctor in clinic may want to perform an abdominal and vaginal examination to try to determine the cause of your infertility. A cervical smear may be taken if this has not recently been carried out and swabs will also be taken to exclude any infection.
Blood tests
There are a number of blood tests you will need to enable us to assess if there is a problem with your hormones. These need to be taken at certain times within your menstrual cycle and you will be told exactly when they need to be taken.
We will also check if you are immune to rubella (German Measles). If you are not immune you will need to have the rubella vaccination and wait a month before you try and get pregnant.
Pelvic ultrasound
This is usually an abdominal ultrasound scan to look at the anatomy of the uterus and ovaries. The scan also includes an assessment of your bladder and kidneys. If it is difficult to assess the pelvic organs from an abdominal approach you may be asked to empty your bladder so that a vaginal scan can be performed.

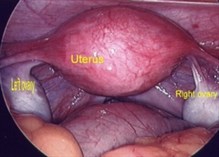
Ultrasound scan showing a normal uterus
You will be asked to drop off a request form at the Radiology Department before you leave the Hospital. An appointment date and time will be arranged and you will receive this in the post along with appropriate instructions.
Cycle tracking/follicle tracking
Cycle/follicle tracking involves a series of internal ultrasound scans and blood tests during your menstrual cycle to determine if and when you ovulate. This is performed by Mrs Moroney and arranged through her secretary by telephone.
Tubal patency tests
It is important that your fallopian tubes are patent as this is where fertilisation of the egg by the sperm occurs. It will depend upon your gynaecology and medical history as to which investigation will be more appropriate and this will be discussed at your consultation.
Hysterosalpingography (HSG)
This is an x-ray of the fallopian tubes and uterus. It is performed in the x-ray department and usually does not require a general anaesthetic. A radio-opaque dye is passed up through the cervix into the uterine cavity, the dye shows up on the x-ray and the doctor is able to see if the dye flows out of both fallopian tubes into the abdominal cavity.

A hysterosalpingogram showing patent fallopian tubes
The test will be discussed at length with you and you will be provided with an information leaflet (which can also be downloaded on this page) to help you arrange the test and advise you of what to expect when you attend for the test.
Laparoscopy
|
|
|
| Laparoscopy of normal pelvis | Blue dye spilling from a normal fallopian tube |
This test should really be regarded as an operation and it requires a general anaesthetic. A slim telescope called a laparoscope is inserted through a small incision made in the abdominal cavity to enable the doctor to see the uterus, fallopian tubes and ovaries. Tubal patency is assessed by Injecting blue dye into the uterus via the cervix. If the tubes are healthy the dye can be seen passing along them and escaping through the outer opening of the tubes.
The test will be discussed at length with you and you will be provided with an information leaflet (Laparoscopy information leaflet) to advise you reasons for performing the test and potential risks of the procedure. If the test is necessary then an admission date will be arranged for you.
Male examination and investigation
Usually you will not be examined in the fertility clinic. If you have any history of a genital problem or there is a problem with your semen analysis then you may, at that stage, need an examination of the testicles to ascertain if there are any abnormalities present.
Semen analysis
You will be asked to produce a semen sample for analysis. It is important that we know a number of things about the sperm you are producing. We need to know the volume and number of sperm you produce, the percentage of sperm moving, the percentage of abnormal sperm and the number of white cell in the sample. A second test may be requested if the first sample is poor as semen samples can vary immensely.
This can be done in the privacy of your own home. It should be produced in the morning after 2 to 5 days of abstinence. You will be given the appropriate container and a request form filled in with your details. You will also be given an instruction leaflet regarding bringing the sample to the laboratory. Essentially the sample should be brought to the laboratory within 2 hours of production, before mid-day on a normal working day. Please ensure that the top of the container is securely in place and that the sample is protected from extremes of temperature while being brought in.
Blood tests
A blood test may be taken to assess your hormone levels and chromosome status in certain types of male infertility.